Antibiotics Aren’t Always The Answer
Since the 1940s, physicians have been prescribing antibiotics to patients with illnesses such as strep throat, the flu and food poisoning. Recently, scientists have discovered that antibiotics may not be “all help and no hurt.” Tiny organisms known as microbes live within human bodies and have adapted to prescribed drugs. Scientists, physicians and patients are working together to slow the process.
According to the Center for Disease Control and Prevention, each year in the United States, “at least two million people become infected with bacteria that are resistant to antibiotics and at least 23,000 people die each year as a direct result of these infections.” Clearly, “antimicrobial resistance,” as the science community calls this issue, is a serious problem.
The main cause for antimicrobial resistance is incorrect prescription by physicians. At least half the time, physicians prescribe antibiotics when unnecessary, or with “incorrect dosing or duration,” according to the Center for Disease Control and Prevention.
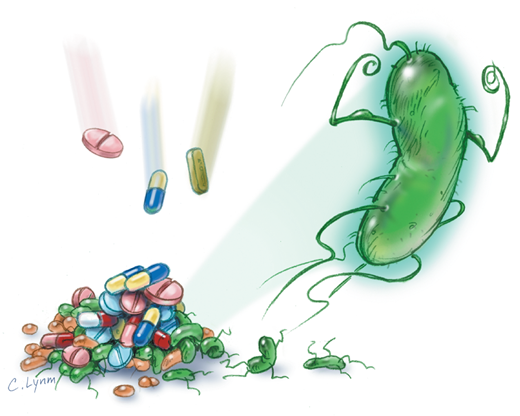
Out of the trillions of bacteria in the human body, some of them are drug resistant, meaning antibiotics will not kill them. The process for how bacteria becomes resistant to antibiotics is rather simple. Once taken, antibiotics kill the bacteria that causes sickness as well as some of the good bacteria. The drug-resistant bacteria remains and spreads its abilities to good bacteria in the body.
“Because antibiotic resistance occurs as part of a natural process in which bacteria evolve, it can be slowed but not stopped,” said the Center for Disease Control and Prevention.
The process cannot be stopped, but it can be slowed in some cases. Practicing the classic hand-washing and coughing into the elbow will help prevent the spread of germs. Also, physicians should only prescribe antibiotics when necessary. Don’t be surprised next time you go to the doctor and leave empty handed; it’s for the best!

Nicole is a senior at St. Dominic High School. She is a peer minister, a member of the Pro-Life Leadership Team, Glamour Gals, Outreach Club and Ambassadors....

